COPD- CHRONIC OBSTRUCTIVE PULMONARY DISORDER

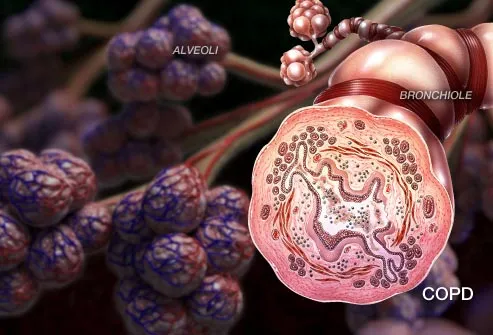
What is COPD?
COPD, or chronic obstructive pulmonary disorder, is a lung disease that makes it hard to breathe. The first symptoms can be so mild that people mistakenly chalk them up to "getting old." People with COPD may develop chronic bronchitis, emphysema, or both. COPD tends to get worse over time, but catching it early, along with good care, can help many people stay active and may slow the disease.
Symptoms of COPD
Inside the lungs, COPD can clog the airways and damage the tiny, balloon-like sacs (alveoli) that absorb oxygen. These changes can cause the following symptoms:
Shortness of breath in everyday activities
Wheezing
Chest tightness
Constant coughing
Producing a lot of mucus (sputum)
Feeling tired
Frequent colds or flu
Advanced Symptoms of COPD
Severe COPD can make it difficult to walk, cook, clean house, or even bathe. Coughing up excess mucus and feeling short of breath may worsen. Advanced illness can also cause:
Swollen legs or feet from fluid buildup
Weight loss
Less muscle strength and endurance
A headache in the morning
Blue or grey lips or fingernails (due to low oxygen levels)
COPD: Chronic Bronchitis
This condition is the main problem for some people with COPD. Its calling card is a nagging cough with plenty of mucus (phlegm). Inside the lungs, the small airways have swollen walls, constant oozing of mucus, and scarring. Trapped mucus can block airflow and become a breeding ground for germs. A "smoker's cough" is typically a sign of chronic bronchitis. The cough is often worse in the morning and in damp, cold weather.
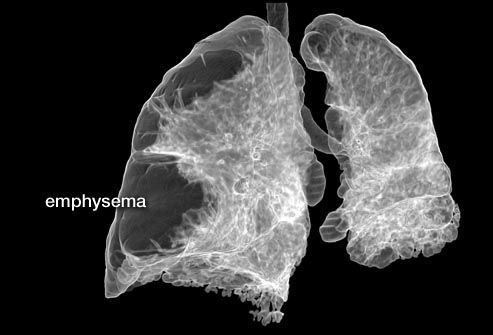
COPD: Emphysema
Emphysema damages the tiny air sacs in the lungs, which inflate when we take in a breath and move oxygen into the blood. They also push out carbon dioxide, a waste gas, when we breathe out. When you have emphysema, these delicate air sacs can't expand and contract properly. In time, the damage destroys the air sacs, leaving large holes in the lungs, which trap stale air. People with emphysema can have great trouble exhaling.
Diagnosis: Physical Exam
First, your doctor will listen to your chest as you breathe, then will ask about your smoking history and whether you have a family history of COPD. The amount of oxygen in your blood may be measured with a blood test or a pulse oximeter, a painless device that clips to a finger.
Diagnosis: Spirometry Breath Test
Spirometry is the main test for COPD. It measures how much air you can move in and out of your lungs, and how quickly you do it. You take a deep breath and blow as hard as you can into a tube. You might repeat the test after inhaling a puff of a bronchodilator medicine, which opens your airways. Spirometry can find problems even before you have symptoms of COPD. It also helps determine the stage of COPD.
Diagnosis: Chest X-Ray
A chest X-ray isn't used to diagnose COPD, but it may help rule out conditions that cause similar symptoms, such as pneumonia. In advanced COPD, a chest X-ray might show lungs that appear much larger than normal.
Treatment: Bronchodilators
Bronchodilators are medications that relax the muscles of the airways to help keep them open and make it easier to breathe. Anticholinergics, a type of bronchodilator, are often used by people with COPD. Short-acting bronchodilators last about four to six hours and are used on an as-needed basis. Longer-acting bronchodilators can be used every day for people with more persistent symptoms. People with COPD may use both types of bronchodilators.
Treatment: Corticosteroids
If bronchodilators don't provide enough relief, people with COPD may take corticosteroids. These are usually taken by inhaler. They may reduce inflammation in the airways. Steroids may also be given by pill or injection to treat flare-ups of COPD.
Treatment: Lung Training
Pulmonary rehabilitation classes teach people ways to keep up with their daily activities without as much shortness of breath. Specific exercises help to build muscle strength, including the muscles used in breathing. You also will learn to manage stress and control your breathing.
Breathing Better With COPD
Pursed-lip breathing can reduce the work of breathing. Breathe in normally through your nose. Then slowly blow the air out through your mouth with your lips in a whistle or kissing position. Your exhale should be longer than the inhale. To strengthen your diaphragm, you can lie on your back on a bed with one hand on your abdomen and one on your chest. Keep your chest as still as possible but let your stomach rise and fall as you breathe.
Treatment: Oxygen Therapy
Severe COPD lowers the oxygen in your blood, so extra oxygen may be needed for your body. It can help you stay active without feeling as tired or out of breath and help protect your brain, heart, and other organs. If you have COPD and need supplemental oxygen, you will typically get the oxygen through tubing from an oxygen tank to the nostrils. Smoking, candles, and other flames are off-limits near oxygen tanks.
Treatment: Antibiotics
People with COPD are at greater risk for lung infections than healthy people. If your cough and shortness of breath get worse or you develop fever, talk to your doctor. These are signs that a lung infection may be taking hold, and your doctor may prescribe medications to help knock it out as quickly as possible. You may also need adjustments to your COPD regimen.
Treatment: Surgery
A small number of people with COPD may benefit from surgery. Bullectomy and lung volume reduction surgery remove the diseased parts of the lung, allowing the healthy tissue to perform better and making breathing easier. A lung transplant may help some people with the most severe COPD who have lung failure, but it can have serious complications.
COPD and Exercise
Walking is one of the best things you can do if you have COPD. Start with just five or 10 minutes at a time, three to five days a week. If you can walk without stopping to rest, add another minute or two. Even if you have severe COPD, you may be able to reach 30 minutes of walking at a time. Use your oxygen while exercising if you are on oxygen therapy. Discuss your exercise plans with your doctor.
What Causes COPD?
About 90% of people with COPD are current or former smokers -- and their disease usually appears after age 40. Second hand smoke and exposure to environmental irritants and pollution also can increase your risk of COPD. In rare cases, the DNA passed down through a family can lead to COPD, even in "never smokers." One of these genetic conditions is called Alpha-1 Antitrypsin (AAT) deficiency.
How Quitting Smoking Helps
Smokers with COPD will lose lung function more quickly. Tobacco smoke destroys the tiny hair-like cilia that normally repair and clean the airways -- and harms the lungs in other ways, too. Quitting will slow or stop the damage, and is simply the most important step you can take for COPD. You'll also get the other benefits of quitting: foods taste better, and your blood pressure and heart rate lower to healthier levels.
COPD and Diet
Being overweight can make it harder to breathe, and being underweight can make you weak. Common guidelines include:
Drink 6-8 glasses of water or non-caffeinated beverages daily.
Eat high-fiber foods such as whole grain bread, bran, and fresh fruit.
Avoid overeating.
Avoid gassy foods such as fried foods, beans, or carbonated drinks.
Eat 4-6 small meals each day.
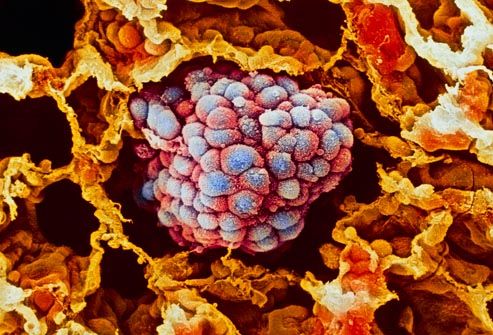
COPD and Cancer
Many people with COPD also develop lung cancer -- likely due to a history of smoking cigarettes. Researchers are studying whether specific genes make some people more vulnerable to COPD or cancer, or both illnesses. Chronic inflammation, caused by smoking or other lung irritants, could play a role in COPD and cancer, as well.
Living With COPD
It’s important to stay active, even if you feel short of breath. You may need to pace yourself or use oxygen therapy, but staying active will make you stronger. Avoid second hand smoke, chemical fumes, and other lung irritants. Be sure to get vaccinated against the flu and pneumococcal disease. Wash your hands frequently, and avoid hacking, sniffling people during cold and flu season. An online community may provide support and practical tips from others with COPD to get the most out of every day.
ps- this is only for information, always consult you physician before having any particular food/ medication/exercise/other remedies.
ps- those interested in recipes are free to view my blog-
http://gseasyrecipes.blogspot.com/
for info about knee replacement, you can view my blog-
http://Knee replacement-stick club.blogspot.com/
for crochet designs
http://My Crochet Creations.blogspot.com/
http://gseasyrecipes.blogspot.com/
for info about knee replacement, you can view my blog-
http://Knee replacement-stick club.blogspot.com/
for crochet designs
http://My Crochet Creations.blogspot.com/
Labels: beans, breathing exercises, bronchodilator, cancer, carbonate, chronic, COPD- chronic obstructive pulmonary disease, diseases, drinks, gassy foods, inflammation, pneumococcal, pollution, Smoking

0 Comments:
Post a Comment
<< Home