Chronic Myelogenous Leukemia

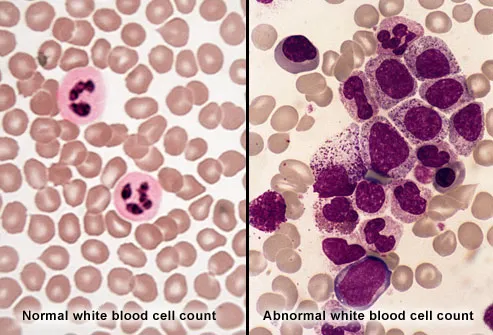
Chronic myelogenous leukemia (also called chronic myeloid
leukemia) is a rare cancer that affects bone marrow. That's
where blood cells are produced. CML leads to the production
of many abnormal white blood cells, which do not fight infection
as well as normal white blood cells. As they build up in the
blood and bone marrow, the abnormal cells crowd out healthy
white blood cells, red blood cells, and platelets.
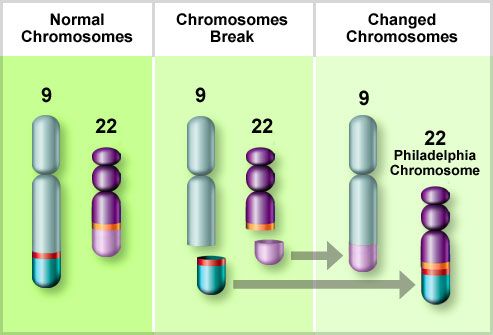
The Philadelphia Chromosome
People with CML have an abnormal chromosome called the
Philadelphia chromosome. Chromosomes carry genes, which
tell cells what to do. In CML, pieces of chromosomes 9 and 22
break and switch places. The changed chromosome 22 is
called the Philadelphia chromosome. It carries a new gene
called bcr-abl. Bcr-abl calls for a protein (tyrosine kinase) to be
made, triggering stem cells to create abnormal white blood
cells found in CML.
Chronic Phase
The chronic phase is the first period of CML.
Most people in this phase don't have any
symptoms. They're usually diagnosed during
a routine blood test. Because there are only a
small number of abnormal white blood cells in
the blood and bone marrow, the body is still
able to fight infection. Even though you might
not feel sick now, it's important to get treated
so CML doesn't progress to the next phase.
Accelerated Phase
During the accelerated phase, you may
develop symptoms such as fatigue, weight loss, shortness of breath, or fever. This means the number of abnormal blood cells has increased. Once in this phase, it may become harder to achieve remission with CML treatments. The accelerated CML phase can lead to the most serious and aggressive phase of the cancer, blast phase.
Blast Phase
By the blast phase of CML, the number of
abnormal blood cells in the bone marrow and
blood is high. Meanwhile, the number of
healthy red and white blood cells and
platelets has dropped. With fewer disease-
fighting white blood cells, you're more likely to
get infections. You may have anaemia or
uncontrolled bleeding. This stage is severe
and life-threatening.
Targeting the Abnormal CML Protein
The chronic phase of CML is first treated with
targeted drugs called tyrosine kinase inhibitors (TKIs). They kill off CML blood cells by blocking the protein produced by the abnormal gene bcr-abl. Side effects can include rashes and swollen skin, nausea, muscle cramps, and diarrhea. When TKIs can't control the disease, there are other treatment options.
Stem Cell Transplant
A stem cell transplant is an option for some
people who don't respond to TKIs. First, you
get high doses of chemotherapy drugs to kill
blood-forming cells (stem cells) in your bone
marrow. Then, you receive stem cells from a
matched donor, called an allogeneic
transplant. These cells will form new, healthy
blood cells. A stem cell transplant is the only
way to cure CML. But newer treatments that
target bcr-abl can also normalize the
Philadelphia chromosome and help many
people with CML achieve remission.
The best candidates for a stem cell transplant:
Are younger rather than older patients
Are in the chronic phase of CML
Are in overall good health
Have a matched stem cell donor (preferably a close relative, such as a brother or sister)
Treatment Options
If TKIs aren't working and you're not a
candidate for a stem cell transplant, other
treatment options include:
Chemotherapy drugs taken by mouth to kill
abnormal cells throughout your body, such as
hydroxyurea or busulfan
Biological therapies, like interferon, that
stimulate your own immune system to fight off
the cancer

Continuous Monitoring Is Necessary
When you have CML, you'll see your doctor at least every few months to monitor treatment and check for side effects. CML tests include:
Complete blood count and bone marrow tests to measure red and white blood cells and platelets
Fluorescent in situ hybridization (FISH) test to see how many cells contain the Philadelphia chromosome
Polymerase chain reaction (PCR) test to look for the bcr-abl gene.
Questions About Your CML Treatment
Here are a few questions to ask your doctor while you're undergoing treatment for CML:
What CML phase am I in?
What are my treatment options and what side effects might I experience?
Should I get a second opinion?
Can I enroll in a clinical trial of an experimental treatment?
How to Cope with CML
During your treatment for CML, here are a few ways to help yourself feel better:
Go to all of your check-ups so your doctor can change treatment if it's not working.
Tell your doctor about any side effects you're experiencing.
If you're struggling with your illness, get support from friends, family members, or your medical team.
Signs Your Treatment Is Working
When you go for regular checkups, your doctor will be looking for these signs that your treatment is working:
Hematologic response: An improvement in the number of healthy white blood cells and platelets
Cytogenic response: Fewer Philadelphia chromosome-positive cells in your blood and bone marrow
You are considered to be in CML remission when:
Your blood cell count is normal (complete hematologic response).
No cells with the Philadelphia chromosome can be found in your blood or bone marrow (complete cytogenic response).
None of the abnormal gene can be found in your blood (complete molecular response).
Being in remission isn't the same as being cured. A stem cell transplant is the only proven cure for CML.
Signs of Relapse
CML can come back even after it has been successfully treated. Signs of relapse include fatigue or weakness, weight loss, fever, night sweats, bone pain, swelling or pain on the left side (a sign of an enlarged spleen), and a feeling of fullness in the belly. If you have any of these symptoms, call your doctor.
Why Isn't My Treatment Working?
CML therapy works well for most people, but not everyone. Reasons why treatment might stop working include:
The cancer cells change (mutate).
Not enough medication is getting into your bloodstream.
If your treatment isn't effective, your doctor may adjust your drug doses or switch you to another therapy.
Labels: chronic myelogenous leukemia (CML), mutation of cells, relapse, Stem Cell Treatment, treatment

0 Comments:
Post a Comment
<< Home